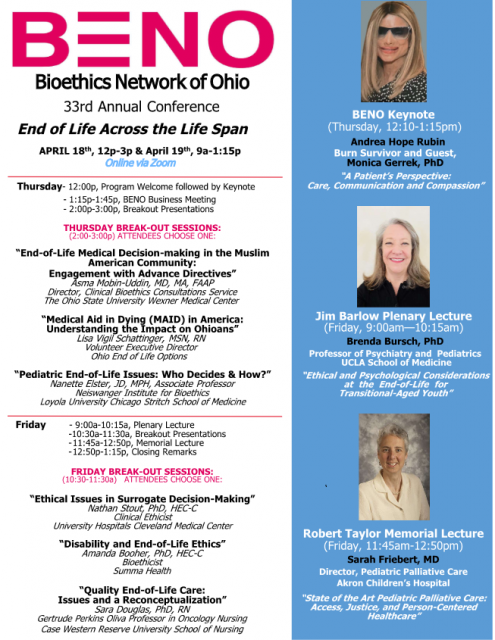
BENO 2024 Conference
THEME:
End of Life Across the Life Span
DATE:
Thursday afternoon, 4/18 and Friday morning, 4/19, all on Zoom
BENO Keynote:
“A Patient’s Perspective: Care, Communication and Compassion”
Andrea Hope Rubin
Burn Survivor and Transformational Speaker
Since her injury, Andrea has been recognized as an inspirational and a much sought-after speaker. The MetroHealth Foundation (Cleveland, OH) awarded her the John A. Gannon Angel Award in 2022. This award is given to a burn survivor who has turned their experience into a way to advocate for others going through similar experiences. She was also the patient of honor at The MetroHealth System’s 2018 biannual gala. In 2019, Andrea was a co-presenter for the John P. McGovern Lecture at the University of Texas Medical Branch-Galveston and her story was highlighted by the American Academy of Ophthalmology. In 2017, she was a member of an esteemed panel on burn ethics at the annual conference of the American Society for Bioethics & Humanities. Andrea has been an invited speaker at the annual meeting of the American Burn Association and has repeatedly been asked to present to medical students and bioethics graduate students. She has also given numerous talks to undergraduate and high school students.
Andrea is the co-author of an article about the problems patients encounter after discharge and was the focus of an article written about ethical issues in burn care. She has been interviewed on podcasts and for newspaper articles. The documentary about Andrea for The MetroHealth System’s Gala won a local Emmy Award.
Monica L. Gerrek, Ph.D.
Assistant Professor, Department of Bioethics, School of Medicine, Case Western Reserve University
Co-Director, Center for Biomedical Ethics, MetroHealth System
Monica L. Gerrek, PhD, is the Co-Director of the Center for Biomedical Ethics at The MetroHealth System, an Assistant Professor in the Department of Bioethics in the School of Medicine at Case Western Reserve University, and a bioethics consultant at Summa Health System. She is also currently chair of MetroHealth’s Ethics Committee and the American Burn Association’s Ethical Issues Committee, and serves on Summa Health’s Ethics Committee. She has a PhD in philosophy and completed the two-year Cleveland Fellowship in Advanced Bioethics offered by Cleveland Clinic, The MetroHealth System, University Hospitals, Cleveland VA, and Case Western Reserve University. Dr. Gerrek has published on topics such as correctional healthcare ethics, ethics in burn care, and animal ethics. She has also given hundreds of presentations, locally, regionally, nationally, and internationally on these topics as well as on topics such as ethics of addiction and clinical ethics. She has won several awards including Case Western Reserve University’s J. Bruce Jackson, MD, Award in Undergraduate Student Mentoring and its School of Medicine’s Faculty STAR Award and was a nominee for the American Burn Association’s 2023 Curtis P. Artz Distinguished Service Award.
Jim Barlow Plenary Lecture:
“Ethical and Psychological Considerations at the End-of-Life for Transitional-Aged Youth”
Brenda Bursch, PhD
Professor of Psychiatry and Pediatrics, UCLA School of Medicine
Dr. Bursch received her PhD from Claremont Graduate School in 1990. She is a Professor in the Departments of Psychiatry & Biobehavioral Sciences and Pediatrics at the David Geffen School of Medicine at UCLA, where she has been on faculty since 1994. She is the Director of the Pediatric Psychology Consultation Liaison service, overseeing consultations for pediatric medical inpatients. Dr. Bursch is a social and medical psychologist with clinical and research interests in pediatric pain, somatization, high health care utilizers, palliative care, and illness falsification. She also has interest and expertise in systems issues (organizational dynamics; patient-family-staff communication; mental wellness and resilience for health care workers; biopsychosocial model). Dr. Bursch has co-authored national guidelines on both Munchausen by Proxy and Pediatric Chronic Pain. She served as an advisor for the DMS-5 section on somatic symptom disorders. She is the co-author of a book entitled ”How Many More Questions?" Techniques for Clinical Interviews of Young Medically Ill Children. And, she serves as a consultant for the Los Angeles County Juvenile Mental Health Court, Los Angeles Lakers, South Bay Lakers, California Conservation Corp, and Lionsgate.
Robert Taylor Memorial Lecture:
“State of the Art Pediatric Palliative Care: Access, Justice, and Person-Centered Healthcare”
Sarah Friebert, MD
Director, Pediatric Palliative Care Division, Akron Children’s Hospital
Dr. Friebert is founder and director of the Haslinger Family Pediatric Palliative Care Center and the Emily Cooper Welty Expressive Therapy Center at Akron Children’s. A graduate of Case Western Reserve University School of Medicine, she completed a residency in pediatrics at the Children’s Hospital of Philadelphia in Philadelphia, Pa. and a fellowship in pediatric hematology/oncology at Rainbow Babies and Children’s Hospital in Cleveland, Ohio. Under her direction, the Haslinger Center features an accredited palliative care fellowship program and has achieved Advanced Certification in Palliative Care from The Joint Commission. Dr. Friebert is also the founding director of the hospital’s addiction services program, which addresses addiction in collaboration with community resources. She is a professor of pediatrics at Northeast Ohio Medical University, where she is also a founding member of the university’s Office of Palliative Care. Board-certified in pediatric hematology/oncology and hospice and palliative medicine, Dr. Friebert is past president of Akron Children’s medical staff and the inaugural chair holder of the Sarah Elizabeth Friebert Pediatric Palliative Care Endowed Chair. She’s also the founder, past chair and ongoing member of the Ohio Pediatric Palliative and End-of-Life Care Network (OPPEN). She is the author of multiple articles and book chapters and is an active research scientist, serving as program director for palliative care research at the Rebecca D. Considine Research Institute. She was co-principal investigator for a Centers for Medicare & Medicaid Health Care Innovation Award, and is principal investigator for multiple palliative care-related research initiatives, Dr. Friebert is also active in multiple local, regional, state and national educational, philanthropic and palliative care organizations.
BENO Breakout Presentations
“End-of-Life Medical Decision-making in the Muslim American Community: Engagement with Advance Directives”
Asma Mobin-Uddin, MD, MA, FAAP
Director, Clinical Bioethics Consultations Service, The Ohio State University Wexner Medical Center
Dr. Asma Mobin-Uddin is a clinical ethicist, pediatrician, and award-winning children’s author. She is the director of the Clinical Bioethics Consultation Service at The Ohio State University Wexner Medical Center and the OSU Center for Bioethics. She is an Assistant Professor in the Division of Bioethics and in the Department of Pediatrics at the OSU College of Medicine, and she is a pediatrician at Nationwide Children’s Hospital. She also serves on the Joint Ethics Advisory Committee for OhioHealth. Dr. Mobin-Uddin was a BENO board member from 2013 – 2022.
Due to an interest in end-of-life ethical dilemmas, Dr. Mobin-Uddin is conducting a research project exploring beliefs about end-of-life medical decision-making in the Muslim-American community. She is working on developing culturally and religiously sensitive educational materials to facilitate end-of-life planning.
Dr. Mobin-Uddin is also the award-winning author of three children’s books about the Muslim-American experience. The New York Times and CNN featured her first book, My Name is Bilal, in articles on how to teach kids to avoid racism and anti-Asian hatred. This book won the Paterson Prize for Books for Young People.
“Medical Aid in Dying (MAID) in America: Understanding the Impact on Ohioans”
Lisa Vigil Schattinger, MSN, RN
Volunteer Executive Director, Ohio End of Life Options
Lisa founded Ohio End of Life Options in 2015. The year before, Lisa was with her stepfather, Dr. Jack Rowe, when he died after using Oregon’s Death with Dignity Act. His death was peaceful and exactly as he had wished. A few months earlier, Jack had been diagnosed with cancer and told he had a few months to live. He enrolled in hospice and communicated openly and honestly with family and friends about his diagnosis. Before he died, he shared his thoughts on the Death with Dignity law in the Journal of the American Medical Association. His family was thankful to be able to surround him with love as he died at home. The experience was profound for Lisa and her family.
After returning home to Cleveland, Lisa shared her family’s experience locally and nationally. It has resonated with many. In 2016, she joined the board of Death with Dignity National Center.
Lisa grew up and went to college in Oregon. After graduating, she worked as a medical assistant in an internist’s office in Eugene. Her mother Jan Rowe was a nurse and they talked about medical issues a lot. They discussed physician-assisted death before it was voted on in 1994. At the time, Lisa’s aunt was being treated for breast cancer, from which she died in 1995. Her aunt was under hospice care but was without the option of medical aid in dying.
Lisa had other experiences with death among friends and family. She found that the concept of quality of life, for those at the end of life, is intensely personal and important. She began working toward a law giving terminally ill Ohioans access to all of their end-of-life options.
“Pediatric End-of-Life Issues: Who Decides & How?”
Nanette Elster, JD, MPH
Associate Professor, Neiswanger Institute for Bioethics, Loyola University Chicago Stritch School of Medicine
Nanette Elster, JD, MPH, is an associate professor at the Neiswanger Institute for Bioethics and Health Policy, Loyola University Chicago Stritch School of Medicine. She is an active educator in the graduate program, teaching a variety of courses in areas related to law, pediatrics, oral health, genetics, and professionalism. She also supervises the graduate program’s writing courses, master capstone course, and doctoral capstone courses.
She has extensive experience in legal, public health and ethical issues related to women’s and children’s health. She has spoken nationally and internationally and is the author of numerous articles on the legal, health policy and ethical implications of a range of public health issues, genetics issues and reproductive issues. She has appeared on such media staples as CNN, Good Morning America, the Today Show, NPR and Chicago Tonight. More recently, she has been quoted in Forbes, Insider, and The Cut.
She served for many years as the chair of the Special Committee on Bioethics and the Law for the American Bar Association and was the Manager of Ethics Outreach for the Council on Ethics, Bylaws and Judicial Affairs of the American Dental Association. She is the legal consultant to the Committee on Bioethics for the American Academy of Pediatrics. She also serves on the board of the Alliance for Fertility Preservation. She was elected in 2016 to serve on the executive board of the Association for Practical and Professional Ethics (APPE). In 2020, she was elected to a two-year term as board member of the Academy for Professionalism in Health Care (APHC); she was re-elected in 2022 for another two-year term serving as Secretary. She is currently a member of the ethics committee of Endeavor Health System and the Ethics Advisory Board of Lurie Children’s Hospital.
In 2017, she received an honorary fellowship to the American College of Dentists. This is bestowed on individuals who do not hold a dental degree but have significantly advanced the profession of oral health and have shown exceptional leadership in areas such as education, research, public health, administration, public service, or related fields of health care. This is the highest honor the ACD awards to non-dentists.
“Ethical Issues in Surrogate Decision-Making”
Nathan Stout, PhD, HEC-C
Clinical Ethicist, University Hospitals Cleveland Medical Center
Nathan Stout is a Clinical Ethicist at University Hospitals Cleveland Medical Center and Clinical Assistant Professor at Case Western Reserve University. He earned his PhD in Philosophy from Tulane University in 2016 and completed a Postdoctoral Fellowship in Clinical Ethics at the Tulane University School of Medicine Program in Medical Ethics and Human Values in 2019. Dr. Stout’s primary research interests are related to issues of moral agency and responsibility and how these are to be understood and interpreted in the context of clinical ethics. His work has appeared in numerous peer-reviewed journals and edited volumes and covers a wide variety of topics in bioethics, moral philosophy, and moral psychology.
“Disability and End-of-Life Ethics”
Amanda Booher, PhD, HEC-C
Bioethicist, Summa Health
Amanda K. Booher is a bioethicist at Summa Health System in Akron, Ohio. She did her bioethics training at Case Western Reserve University and Metrohealth Hospital System. Prior to that, she was an English professor specializing in the rhetorical, theoretical, and medical relationships of bodies and prosthetics, with publications in journals including Disability Studies Quarterly and the International Journal of Feminist Approaches to Bioethics.
“Quality End-of-Life Care: Issues and a Reconceptualization”
Sara Douglas, PhD, RN
Gertrude Perkins Oliva Professor in Oncology Nursing, Case Western Reserve University School of Nursing
Sara Douglas, PhD, RN is the Gertrude Perkins Oliva Endowed Professor in Oncology Nursing at the Frances Payne Bolton School of Nursing, Case Western Reserve University and holds a secondary appointment at the School of Medicine at Case Western Reserve University. She received her undergraduate degree in nursing at the University of Kentucky, her Masters’ Degree from the University of Pennsylvania, and her PhD from Illinois State University. She has been a faculty member in the Frances Payne Bolton School of Nursing since 1991. She has a 20+ year history of conducting research focused on patients with life-limiting illness and their caregivers. Dr. Douglas’ research has focused on treatment decisions made by patients with life-limiting illnesses and in the past 10 years had focused primarily on end-of-life decision making by patients with advanced cancer and their caregivers. Her work has appeared in the New York Times, as well as prominent scientific journals (JAMA Network Open, Journal of Clinical Oncology Practice, Palliative and Supportive Care). She recently received a 5-year National Cancer Institute/NIH grant to study dyadic quality end-of-life in patients with advanced cancer and their caregivers.
Videos
Registration is closed
Home | Bio-Quarterly | Membership | Videos | Officers | Trustees | Resources | Contact | Bylaws
Bioethics Network of Ohio | 22425 Canterbury Lane | Shaker Heights, Ohio 44122 | Phone: 216-403-2430
All Rights Reserved 2024, Bioethics Network of Ohio - Admin Login | Web Design by Alt Media Studios